People often offer Ten Commandments for helping those living with Alzheimer’s disease or dementia, in which every command begins with the word “Never.”
But because being positive and avoiding saying “no” can be key in creating more easygoing conversations with people who have dementia – and because they hate being told not to do things – we’ve created a more positive list of commandments.
This is the approach that is encouraged by Shannon Braun, director of ERS’ Center for Memory Support and Inclusion.
Not focusing on the negative
“I had one person, years ago, in one of my support groups, say that they felt like the list is negative because they all start with ‘never,’ Braun said. “They tell you what not to do first. While it’s true information, it’s kind of telling you, ‘No, don’t do that. Do this instead.’”
So here are our suggested Ten Tips for communicating with people who are living with forms of dementia:
1. Almost always agree with them (An exception: when they believe something unsafe). Two techniques that are helpful with this are the use of Improv techniques, and the use of “the 3 R’s” -- Right, Reassure, Redirect. Right means acting as if what they’re saying is absolutely true. Don’t try to correct them, because people with dementia will probably dig in their heels and insist what they’re saying is accurate. Arguing is usually futile. After we’ve agreed on their reality, we can provide comforting reassurance (the second R) to the person living with dementia. After that, we can redirect the topic of conversation (the third R), perhaps by asking a question about something else or moving to a new environment.
2. Reminisce with them. If they’re having a moment where they are hoping their mother or father will pick them up from school today, ask them about Mom or Dad, and what they were like. This is much more pleasant than telling them their parents died long ago, and re-triggering the mourning process for them. Reminiscing with them is far more comfortable for them than asking them, “Do you remember…?” Because chances are, they don’t, and few people enjoy being quizzed. “When I work with care partners, we talk about how each person’s memory is like their diary,” Braun said. “Our job is to meet them on that page, rather than trying to lead them to be oriented toward to the reality of your own diary page, in the present day.”
3. Repeat requests – pleasantly – that you have made of them. If they haven’t done something you asked of them, state your request again, pleasantly, as if you never had asked it, instead of chiding them for failing to comply. “Can you please take those pills on the table?” is much nicer than, “I told you to take those pills.”

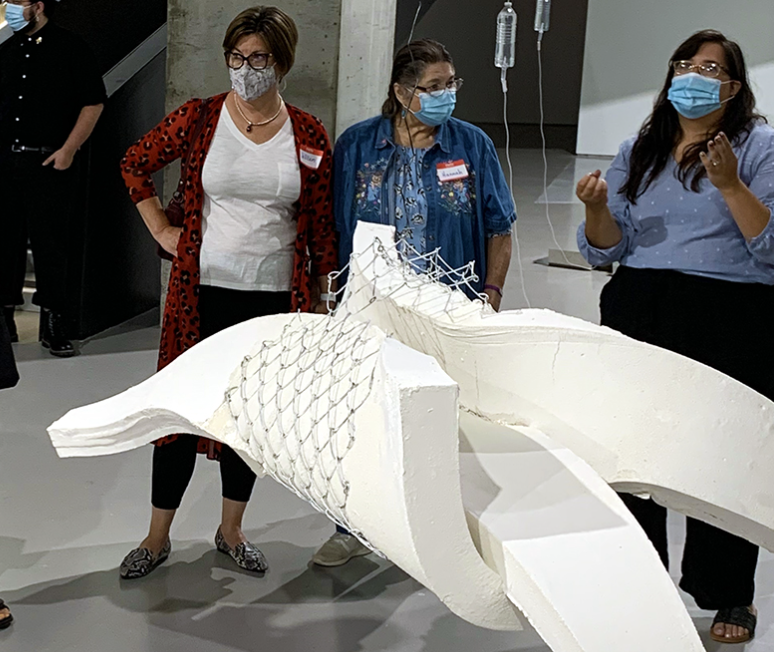
Above: Shannon Braun, director of ERS' Center for Memory Support and Inclusion
4. Focus on what your loved one can do, rather than what they can’t. Part of the dementia journey is a loss of independence, which is something they’re quite aware of. They feel the constraints of not being able to do things, and hate frequently being told ‘no,’ or ‘don’t.” So instead of saying “You can’t,” search for the things they can do successfully, and encourage them to gravitate to them.
5. Distract them if they’re doing something inappropriate, rather than shaming them. People with Alzheimer’s disease or dementia sometimes do inappropriate things, such as cursing, making sexual comments, or hurtful (including prejudiced or offensive) comments. They may not realize their comments are inappropriate.
6. Ask --- and model behavior – instead of demanding things. As we know, actions can speak more eloquently than words. If your loved one isn’t realizing your sense of urgency, it can be very helpful to do what you want them to do. If you’d like them to start eating, take a few bites of food yourself, with hope they will imitate you.
Related: If you're a care partner for someone living with dementia, ERS' Center for Memory Support and Inclusion (CMIS) has programs at several museums, the Cincinnati Zoo, and a dance studio that allow you to spend stress-free time with your loved one. Click here to visit our CMSI website to learn more.
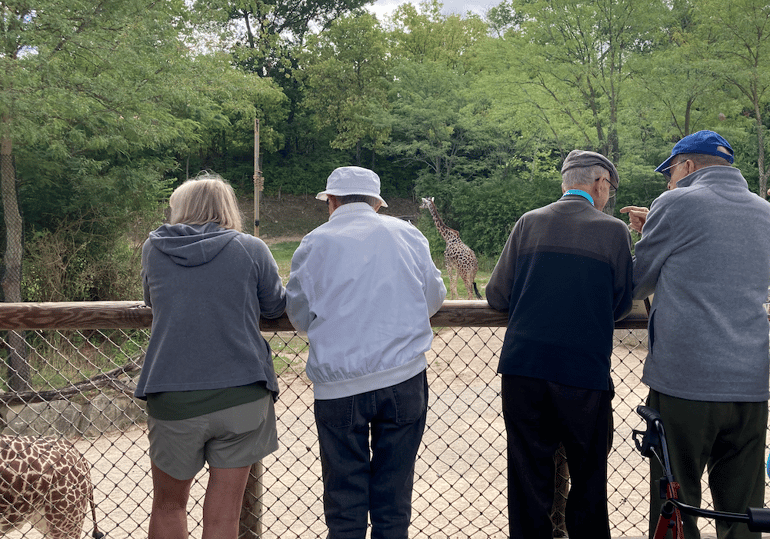
Above: Participants in the Wild About Minds program, presented by ERS' Center for Memory Support and Inclusion, and the Cincinnati Zoo.
7. Involve your loved one in conversations, including about their health and well-being. Don’t speak with others as if your loved one isn’t there. This can hurt their feelings, for obvious reasons, and can lead them to be angry toward the care providers you’re speaking with. Position yourself so they’re an obvious part of the conversation and more than welcome to speak.
8. Pay attention to them while speaking with them, and avoid being condescending. “We have to be aware of our language, but not just our verbal language – the way we’re communicating with non-verbals, the way our faces are interacting, with smiling, eye contact, not looking at your watch,” Braun said. “Be present.”
9. Empathize with them, and sometimes match your loved one’s energy. “I think if someone is really upset, you can try to not make matters worse, but kind-of match their energy,” Braun said. “You’re in it with them, and then you can calm down together. If someone is panicked, you understand the panic, you’re empathizing and you’re validating it. And then, you’re reassuring, and redirecting.”
10. Always remember: They’re doing the best they can. We mention this one last – although it’s arguably the most important – because we want you to never forget
that even when they’re being ornery, cranky, or stubborn, and not doing what you asked of them, they probably are struggling to do what you have asked – or they forgot.
We hope this is helpful for you and your care partner. We know how difficult the journey can be. We also hope you find treasured moments with your loved one as you provide care. If you aren’t, perhaps a friend or family member can fill in for a while to provide respite for you.